How is HLH treated?
Firstly the aim for treatment is to reduce the severe excessive inflammation that is responsible for the life-threatening symptoms.
Secondly, treatment aims to kill any of the immune cells that have been infected by a trigger, for example viruses and bacteria. This aims to remove the trigger for the excessive inflammation.
Unfortunately, even if the original infection that triggered the HLH is killed, that is not enough to stop the excessive inflammation, since it has spiralled out of control.
Thirdly, the ultimate aim for children with a genetic cause of HLH is stem cell transplantation. This aims to replace the defective cells in the bone marrow, with healthy cells from a donor.
Treatment is tailored for individual patients, and is guided by the type of HLH your child has, the severity of the severity of the symptoms, the age of the patient, and any other underlying conditions
As HLH is uncommon and serious, treatment is usually coordinated by a specialist centre experienced in treating rare immune disorders.
The priority of treatment is to damp down (suppress) the immune system to reduce the over-reaction and lessen the risk of tissue damage. This will often involve courses of corticosteroids and chemotherapy medicines, usually given into a vein (intravenously) in hospital. Some of the medicines used are listed in the table below but new treatments are being developed all the time. Treatment will be individualized to minimise side effects, which your medical team will discuss with you. If an infectious trigger is suspected, anti-infection treatment may be given, such as antibiotics or other medication.
Type of drug: Example: How it is given
Steroid: Dexamethasone, prednisolone: Daily injection into a vein or by mouth
Calcineurin inhibitor: Cyclosporin: Twice daily, into a vein or by mouth
Cytotoxic chemotherapy: Etoposide: Into a vein, twice weekly at first then less often over time
Methotrexate: By injection into the fluid around the spinal cord, up to four doses weekly if the brain is affected
Biologics: Alemtuzumab: Into a vein, daily for a few days
In the case of primary HLH, this treatment usually puts the condition into remission, but the risk of relapse remains.
Corrective treatment of HLH
In many cases, haematopoietic stem cell transplant (HSCT, including bone marrow transplant, or BMT) offers the potential for long-term cure of primary HLH. HSCT aims to replace the faulty immune system with an immune system from a healthy donor. Stem cells, from which all the cells of the immune system develop, can be obtained from healthy bone marrow, or in some cases from umbilical cord blood or donor blood. The healthy stem cells can be given by transfusion into a vein to a child with HLH.
he symptoms, the age of the patient, and any other underlying conditions.
HLH Treatment Protocol
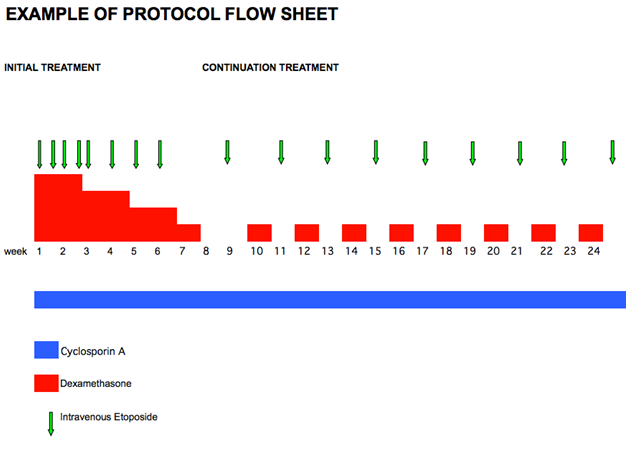
The vast majority of children with HLH will be treated with chemotherapy and immunotherapy guided by an international protocol (see example below), which maps out the dates for the different medications. The protocol will be tailored to your child.
If your child needs chemotherapy, he or she will probably need a central line. This is a tube that is inserted into a large blood vessel and tunnelled under the skin to where it can be easily accessed. It allows blood samples to be taken and treatment, including chemotherapy, to be given easily and painlessly. The central line is put in under general anaesthesia and will stay in place until the end of your child’s treatment. Your hospital will provide more information about the types of central lines they offer.
If your child is unwell or requires more intensive treatment he or she will need to be in hospital. Some children however receive some of their intravenous treatment by visiting their hospital out-patient or day-care facility. This may only be available at your treating oncologist/haematologist’s hospital or at your local hospital under a shared care arrangement with a local doctor. Some treatment, like that taken by mouth, can be given at home.
While on chemotherapy, for up to 6 months afterwards, and up to a year after a bone marrow transplant, your child will be susceptible to infections. This is known as being immunocompromised. If he or she develops a fever or becomes unwell you need to contact your treating team immediately for advice. Your child may need immediate hospital admission and treatment with antibiotics.
What are the side-effects of the Treatments?
The main drugs used to treat HLH and their common side effects are described below.
Steroids:
Dexamethasone/prednisolone – these are corticosteroids (steroids) that can reduce inflammation and suppress the immune system. They are usually given by mouth, in the form of pills, pills that dissolve in water, or as a liquid medicine.
There are a number of known possible side effects. You will not necessarily experience all of these.
Possible side-effects include: irritation of the stomach lining (indigestion/discomfort/pain), increased appetite, weight gain, changes in behaviour (mood swings/difficulty in sleeping/anxiety/irritability), temporary increase in blood-sugar level (like someone with diabetes), high blood pressure, increased risk of infection due to suppression of the immune system, impaired wound healing, irregular or absent periods, and inflammation of the pancreas. Long-term steroid use may also cause muscle weakness, a reduction in bone density (bones become more fragile), cataracts and growth failure.
Chemotherapy:
Chemotherapy is a drug usually used to treat cancer but some chemotherapy drugs are also very effective against HLH. These drugs work by killing cells that are dividing and reproducing themselves.
Different chemotherapy drugs cause different side effects. Everyone is different and will react to chemotherapy treatment in a different way. Some patients may have very few side effects while others will have a lot. Almost all side effects are only short-term and will gradually disappear once the treatment has stopped.
The main areas of your body that may be affected by chemotherapy are those where normal cells rapidly divide and grow. Examples include the lining of the mouth causing a sore mouth, the digestive system causing diarrhoea, skin and hair, causing hair loss, and the bone marrow (spongy material that fills the bones and produces new blood cells), causing low blood counts.
There are three main types of blood cells that might be affected:
• Red blood cells which carry oxygen around the body
• White blood cells which fight infections
• Platelets which help to clot the blood to prevent bleeding and bruising
Chemotherapy reduces the production and therefore, the number of blood cells in the body. Too few red blood cells cause anaemia, and the person becomes tired and pale. If there are too few white blood cells, particularly those called neutrophils (neutropenia), the person is at increased risk of infection. Too few platelets means the person is at increased risk of excessive bleeding when injured, having nose-bleeds or bruising easily. If the counts get really low, you may need a red cell transfusion or platelet transfusion. Transfusions are also needed to support those patients who undergo intensive chemotherapy.
As the chemotherapy affects your immune system, you may need antibiotics to help fight any infection. This means if you have a temperature of 38°C or more, or becomes unwell (even with a normal temperature) you must go to hospital where you may have to stay for a couple of days whilst being given antibiotics. You may also have to avoid giving paracetamol or ibuprofen until you are reviewed in hospital, as these drugs lower high temperatures and can potentially mask an infection. In addition, if you are in contact with someone who has chickenpox, shingles or measles, then you should let your hospital know as these are dangerous infections for a patient with a low (suppressed) immune system. Both you and the rest of your family should have the annual flu jab during the autumn/winter.
Chemotherapy can also cause nausea and vomiting, but anti-sickness medicines known as anti-emetic drugs can control this side effect.
Hair loss can occur, but this does not always happen with the chemotherapy used to treat HLH. Young patient often get used to hair loss fairly quickly but for others it is far more traumatic, fortunately, all hair loss from chemotherapy is temporary and hair growth returns once treatment has stopped.
Fertility may be affected, depending on which chemotherapy drugs you receive. You should discuss your particular treatment with your oncologist/haematologist for more information.
Other side effects are an increased sensitivity to the sun, so you should keep out of intense sunlight and use sun block.
Treatment Centres
Haemophagocytic Lymphohistiocytosis is a rare disease. Treatment and full investigation are performed at specialist treatment centres that have experience with dealing with patients with HLH and the specialist medications. There are specialist centres in the UK which treat cancer and rare diseases and you care will be co-ordinated from there. To make things a bit easier for your family, you may receive some treatment in a hospital local to your home (shared care), but the overall management plan for your treatment will ultimately be undertaken from your closest treatment centre.
Complementary (Alternative) Therapies
In the past, many doctors dismissed alternative or complementary medicine, but it is now recognised that families often benefit from the positive effects of treatments such as acupuncture, massage, counselling or nutritional therapy.
Several effective chemotherapy drugs are derived from natural sources, especially fungi and plants. The main ‘problem’ with complementary therapy is that individual treatments are hardly ever subjected to the same intense scrutiny and ‘clinical trials’ as official drugs, and that is a matter of considerable concern. It is therefore, important that you discuss with your consultant any of the alternative therapies you plan to use, to ensure that they do not interact in any harmful way with your medication. Herbal ‘remedies’ are a case in point, since some of them are known to interfere with medically prescribed drugs proven to help. The following are just some of the over-the counter treatments that interfere with the action of chemotherapy drugs, or other medicines such as antibiotics: bilberry; Echinacea; fish oils; garlic; glucosamines; meadowsweet; selenium and St John’s wort.
Please be advised that all the information you read here is not a replacement for the advice you will get from your consultant and their team.
Help ensure that we can continue to bring you this vital informational material, make a donation today
